Background: Cytokine release syndrome (CRS) is a supraphysiologic response to T-cell engaging immunotherapy that can negatively impact the treatment experience of patients with non-Hodgkin lymphoma (NHL) and other blood cancers. We explored patient, caregiver and healthcare professional (HCP) perspectives on key burdens and unmet needs associated with CRS.
Methods: Existing insights from disease-level patient journeys (follicular lymphoma, diffuse large B-cell lymphoma, multiple myeloma [MM]) and reports from focus groups with a CRS patient working group from the USA, UK, Canada, and Belgium were assessed to identify key questions. Further interviews were conducted (November 2022-January 2023) in the USA, UK, Germany, and Austria to address these questions with patients, caregivers and HCPs. HCP insights were collected via 60-minute virtual interviews; patient and caregiver insights were collected via video homework tasks and 60-minute virtual interviews. Outputs were validated by the working group, consisting of patients with CRS experience and representatives of patient organizations.
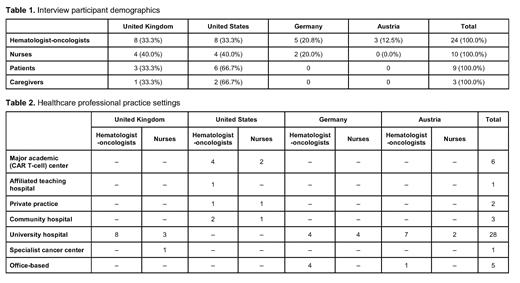
Results: A total of 34 HCPs (hemato-oncologists, n=24; nurses, n=10; Tables 1 & 2) with varying degrees of experience of managing CRS were interviewed, along with 9 patients and 3 caregivers (associated diagnoses: NHL, n=6; MM, n=5; acute lymphocytic leukemia, n=1). All patients had experienced CRS (Grade 1-3) as a result of CAR T-cell (n=6) or bispecific antibody (n=3) therapy.
Insights were based on five focus areas: 1) patient education and information; 2) CRS diagnosis and management; 3) CRS in different healthcare archetypes; 4) digital literacy and the role of technology in mitigating/monitoring/managing CRS; and 5) the caregiver perspective.
CRS education was a primary unmet need, but overall awareness and knowledge of CRS was strong among the patient sample. Patients noted the life-threatening potential of CRS, but preferred to be on active treatment. HCP communication to patients focused on CRS being an expected occurrence rather than a marker of treatment failure, the need for in-patient admission in some cases and/or close monitoring, and the critical role of caregivers.
Generally, HCPs were familiar with CRS and the procedures for its monitoring and management, but the variability in time to onset, severity of symptoms, and potential impact on quality of life (QOL) warranted caution. Logistics emerged as a common barrier, with CRS treatment often administered at major hospitals, as local, community-based clinics do not currently have the required capacity/capability to manage CRS; this could be achieved via the provision of training and support. Uncertainty remains regarding the broader roll out of bispecific antibodies, given the variability in CRS treatment between countries.
Patients, HCPs and caregivers were aligned on their preferences for remote monitoring for CRS. All three groups expressed the need for simple, easy-to-use solutions that integrate seamlessly with existing systems and do not cause undue concern with false alarms, complex technical set-up and patient user experience. Patients emphasized the need for prompt and assured access to their medical team in case of an emergency. HCPs expressed a range of opinions on the feasibility of adopting such solutions. Some were open to using new tools and saw the potential for alleviating resource challenges. Others had reservations about interoperability and questions around over-informing patients with detailed data. Patients were open to adopting new technologies, if they added tangible benefit to their QOL, avoided additional logistical burden and improved their experience.
Conclusions: There is strong awareness among patients, caregivers, and HCPs of the risks associated with CRS and the potential impact on QOL. HCPs with experience in administering cellular immunotherapies are confident in monitoring and managing CRS; however, its unpredictability and logistical burden need to be addressed. There is value in adopting digital solutions for CRS monitoring and management. Concerns remain around interoperability, data stewardship, and integration and validation within current hospital systems. Patients' concerns regarding the useability of such digital solutions and assured data privacy also need to be addressed as part of solution development in the CRS space.
Disclosures
Soong:F. Hoffmann La Roche Ltd: Current Employment; GSK plc: Ended employment in the past 24 months. De Carlo:F. Hoffmann La Roche Ltd: Current Employment. Lasi-Tejani:Genentech, Inc. (subsidiary of Roche): Current Employment; F. Hoffmann-La Roche Ltd/Genentech, Inc. only through current compensation package: Current equity holder in publicly-traded company. Sethi:F. Hoffmann La Roche Ltd: Current Employment. Elias:Myeloma Canada: Current Employment; Janssen, AbbVIe: Consultancy; International Myeloma Foundation: Membership on an entity's Board of Directors or advisory committees. Clavreul:Myeloma Patients Europe AISBL (MPE): Current Employment; MPE has participated in paid advisory boards with the following companies in 2022-2023: Roche, Janssen, Pfizer, Takeda, Menarini.: Membership on an entity's Board of Directors or advisory committees; MPE is receiving funding from the following companies: https://www.mpeurope.org/about- mpe/our-funding/: Other. Chandler:F. Hoffmann La Roche Ltd: Current Employment; F. Hoffmann La Roche Ltd: Current equity holder in private company; F. Hoffmann La Roche Ltd: Patents & Royalties. Finzler:F. Hoffmann La Roche Ltd: Current holder of stock options in a privately-held company. Nouet:F. Hoffmann La Roche Ltd: Current Employment, Current equity holder in publicly-traded company, Divested equity in a private or publicly-traded company in the past 24 months. Del Santo:F. Hoffmann La Roche Ltd: Current Employment.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal